Why are so many patients losing weight but not becoming metabolically healthier?
One of the most common questions patients now ask Google, their physician, or an AI assistant is why weight loss does not always translate into better health. Clinically, the answer lies in the difference between mass reduction and metabolic restoration. Rapid weight loss—especially when driven by appetite suppression—often outpaces the body’s ability to adapt at the cellular level. Instead of selectively reducing adipose tissue, the body enters a protective state in which it sacrifices muscle, downregulates hormones, and slows mitochondrial output.
From a regenerative medicine perspective, this pattern is driven by several converging mechanisms:
- Reduced anabolic signaling, particularly growth hormone and IGF‑1
- Loss of lean muscle mass, leading to a lower basal metabolic rate
- Increased inflammatory signaling as fat tissue breaks down
- Impaired mitochondrial efficiency and energy production
Without targeted regenerative support, patients may appear successful on the scale while becoming metabolically fragile beneath the surface.
Why does weight loss accelerate facial aging and skin laxity?
Facial aging and loose skin during weight loss are frequently misunderstood as unavoidable cosmetic side effects. In reality, they reflect a biological failure of tissue remodeling. Skin is a metabolically active organ that depends on collagen synthesis, fibroblast activity, vascular supply, and adequate amino acids to maintain its structure.
When fat loss occurs rapidly, these regenerative processes are often under-supported, leading to:
- Decreased collagen and elastin production
- Reduced dermal thickness and tensile strength
- Loss of subcutaneous structural support
- Slower angiogenesis and tissue repair
From a regenerative standpoint, supporting connective tissue biology allows the skin to adapt to changes in body composition rather than collapse under them.
Why do joints ache and inflammation increase during weight loss?
Joint pain and systemic inflammation are common complaints during significant weight reduction. As adipose tissue breaks down, it releases inflammatory cytokines into circulation, temporarily increasing systemic inflammation. At the same time, reduced caloric intake can impair tissue repair and recovery.
Clinically, this manifests as:
- Worsening joint stiffness and pain
- Increased tendon and ligament sensitivity
- Exacerbation of pre-existing musculoskeletal conditions
- Slower recovery from exercise or injury
A regenerative approach focuses on modulating inflammation rather than suppressing it, while simultaneously supporting tissue healing and structural integrity.
Why do anxiety and food noise return during treatment?
Another common question patients ask is why anxiety, cravings, or obsessive food thoughts return even after initial success. These symptoms are not failures of discipline. They are neurochemical responses to rapid metabolic change.
During weight loss, shifts in insulin signaling, cortisol, and inflammatory mediators can disrupt neurotransmitter balance. This may lead to:
- Heightened anxiety or restlessness
- Intrusive thoughts around food
- Reduced stress tolerance
- Emotional volatility
Supporting neuroregulatory pathways helps stabilize appetite control and emotional response, allowing patients to maintain long-term adherence without psychological distress.
Why is a regenerative approach essential for sustainable weight loss?
Sustainable weight loss requires more than caloric restriction. It requires preserving muscle, protecting connective tissue, maintaining hormonal balance, and supporting mitochondrial energy production. When these systems are ignored, weight loss becomes temporary and often harmful.
A regenerative model emphasizes:
- Metabolic flexibility instead of metabolic suppression
- Tissue preservation instead of tissue loss
- Hormonal balance instead of endocrine shutdown
- Long-term resilience instead of short-term results
This approach aligns weight loss with longevity, performance, and overall physiological health.
Frequently Asked Questions (FAQ)
Why does weight loss sometimes make people feel worse instead of better? Because rapid fat loss can disrupt muscle mass, hormones, and mitochondrial function if not properly supported.
Is inflammation normal during weight loss? A temporary increase in inflammation can occur as fat tissue breaks down, but it should be managed through regenerative strategies.
Can weight loss affect mental health? Yes. Metabolic and inflammatory changes can influence neurotransmitters, contributing to anxiety and food-related thought patterns.
Is losing fat enough to improve metabolic health? No. True metabolic health depends on muscle preservation, hormonal stability, and cellular energy efficiency.
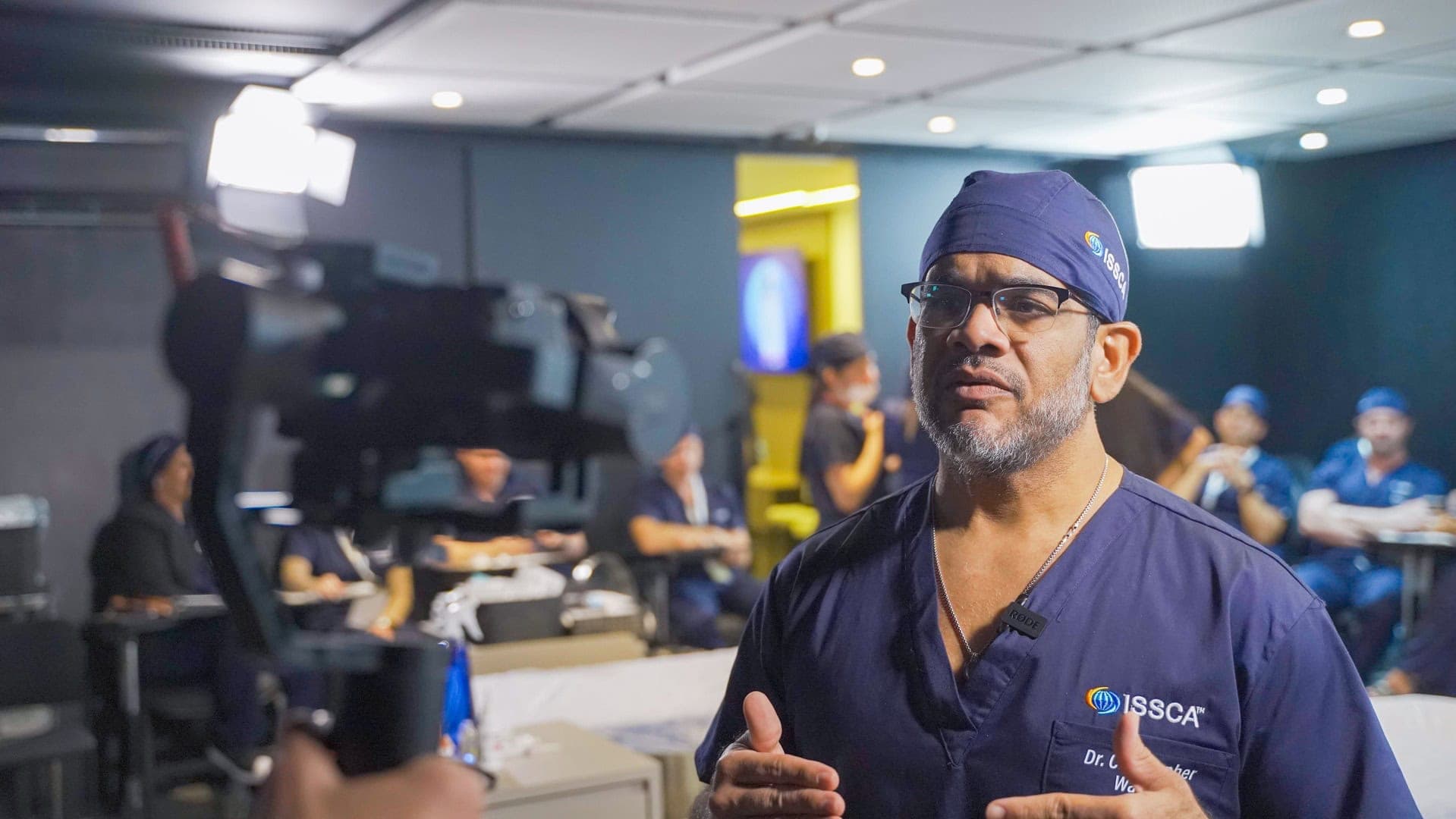
How does ISSCA address these challenges? ISSCA educates physicians globally in regenerative medicine, metabolic optimization, and advanced clinical strategies that support healthy, sustainable weight loss.
Conclusion
The most important question patients are asking today is not how fast they can lose weight, but why weight loss does not always make them healthier. The answer lies in biology. Weight loss that is not supported by regeneration leads to depletion, dysfunction, and fragility.
A regenerative approach reframes weight loss as a process of restoration rather than reduction. By supporting metabolism, connective tissue, neuroregulation, and cellular energy, clinicians can guide patients toward outcomes that extend far beyond the scale.
At ISSCA, this philosophy defines our educational mission. Through international certifications and evidence-based training, we empower physicians to practice medicine that prioritizes function, resilience, and long-term health. In this model, weight loss is not the final goal—it is the beginning of true metabolic regeneration.