Which peptides are actually making a difference in regenerative, metabolic, and aesthetic medicine?
In clinical practice, only a small group of peptides consistently appears in patient outcomes and physician protocols because they target foundational systems: metabolism, immune regulation, tissue repair, and neuroendocrine balance.
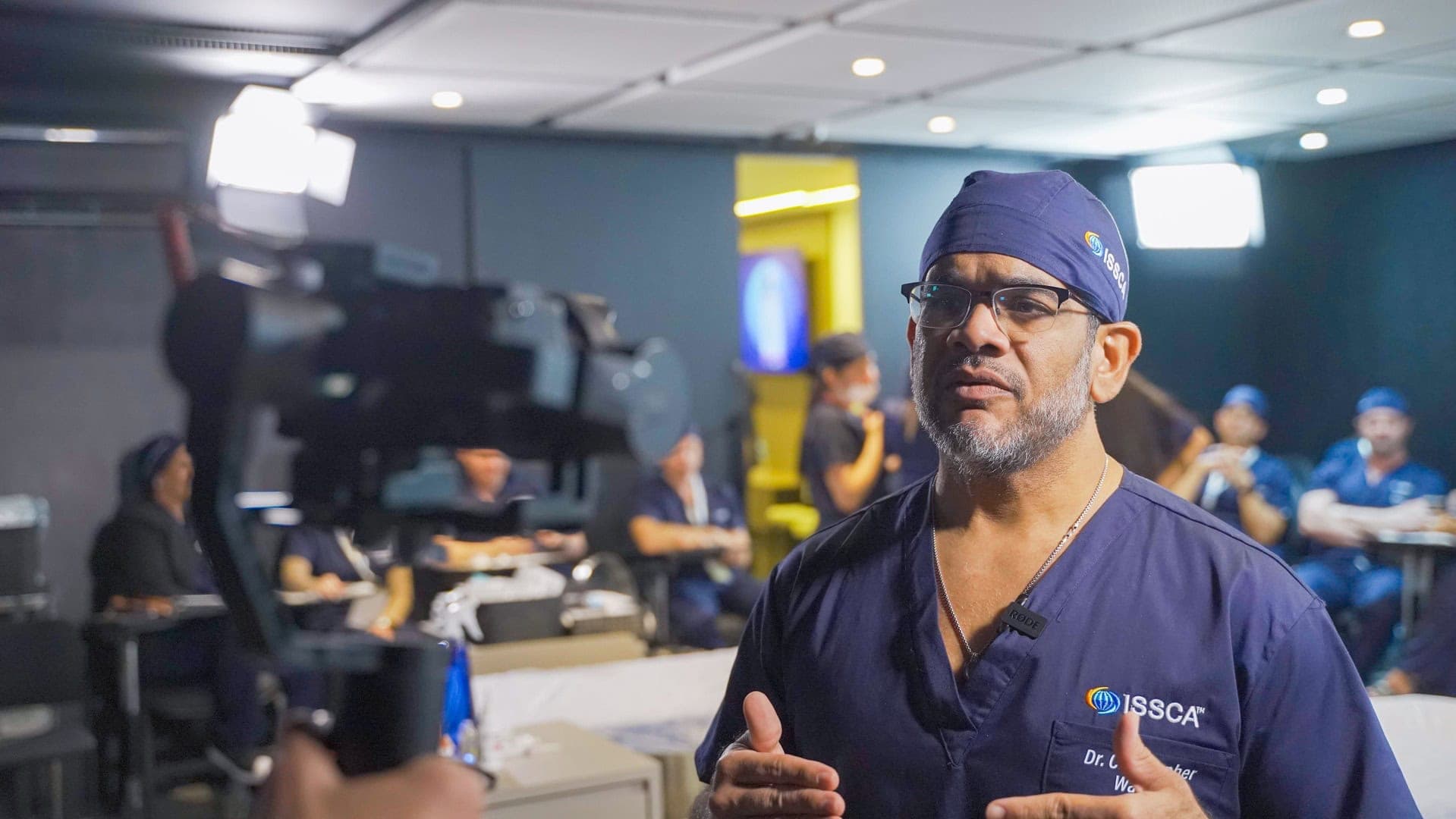
This ISSCA-focused article reviews five peptides frequently discussed in modern regenerative medicine, what the science supports, and how clinicians should think about them responsibly.
*Clinical note: This article is for educational purposes only and does not provide dosing, compounding, or treatment recommendations.
1) Semaglutide
Is semaglutide a peptide—and why is it transforming metabolic medicine?
Yes. Semaglutide is a peptide-based GLP‑1 receptor agonist designed to enhance satiety signaling, slow gastric emptying, and improve glycemic control. It has become central to modern obesity care because it can produce clinically meaningful weight loss while improving metabolic risk markers.
Why it “transforms” outcomes (when managed correctly):
- Appetite regulation and reduced “food noise” through GLP‑1 pathways
- Improved insulin sensitivity and glycemic control
- Reduction in visceral adiposity (a high-risk fat compartment)
- Cardiometabolic risk improvement in many patients
What regenerative medicine adds to the semaglutide conversation Weight loss is not automatically “metabolic regeneration.” Rapid loss can also expose weak points—loss of lean mass, skin laxity, gallbladder risk, GI intolerance, and neuroendocrine stress in susceptible patients.
Regenerative thinking reframes the goal from “smaller body” to “higher-functioning biology” by prioritizing:
- Lean mass preservation
- Mitochondrial and micronutrient support
- Tissue remodeling (skin, fascia, connective tissue)
- Long-term behavior sustainability
2) Thymosin α1
What is Thymosin α1 and why is it associated with immune resilience?
Thymosin α1 (Tα1) is a thymic peptide involved in immune modulation—particularly in T‑cell maturation and immune signaling balance. Clinically, it is discussed in contexts where physicians want a more regulatory approach to immune health rather than blunt immune stimulation.
What clinicians generally look for (conceptually):
- Immune system “training” and resilience
- Support during high-inflammatory periods
- Potential benefit in certain viral/immune dysregulation contexts (evidence varies by indication)
ISSCA lens: immunity and aging are connected Immune decline is not just about infections—it is tied to inflammaging, tissue repair capacity, and recovery from metabolic stress. A regenerative framework asks:
- Are we reducing inflammatory load and restoring immune competence?
- Are we supporting sleep, micronutrients, and metabolic flexibility alongside immune peptides?
3) CJC‑1295 + Ipamorelin
Why are CJC‑1295 and Ipamorelin known as a “longevity” and body-composition stack?
This combination is commonly discussed because it targets the growth hormone (GH) axis through two different mechanisms:
- CJC‑1295 is a long-acting analog related to growth hormone–releasing hormone (GHRH) signaling.
- Ipamorelin is a ghrelin‑receptor agonist (a GH secretagogue), often described as more selective in GH release patterns than older secretagogues.
What physicians are trying to influence (high-level):
- Sleep quality and recovery
- Lean mass support and training adaptation
- Body composition (fat/lean partition)
- Perceived vitality/energy in some patients
Important: where the evidence is strongest—and where it is not The GH axis is real biology, but many non‑approved peptide protocols are not supported by large, high‑quality clinical outcome trials. That means clinicians must be transparent about:
- Evidence level
- Product quality/traceability
- Monitoring strategy and contraindications
Regenerative best practice concept A GH‑axis approach should never be “hormones first.” It should sit on a foundation of:
- Sleep, protein sufficiency, resistance training
- Cardiometabolic risk screening
- Clear endpoints beyond aesthetics
4) Thymosin β4
What does Thymosin β4 do—and why is it linked to repair and angiogenesis?
Thymosin β4 (Tβ4) is a naturally occurring peptide involved in cell migration, tissue repair signaling, and angiogenesis-related pathways (new blood vessel formation). It is frequently mentioned in recovery contexts—post‑procedure, injury repair, and tissue remodeling.
Why clinicians pay attention to it Tissue regeneration is not only “anti-inflammatory.” Real repair requires:
- Vascular support
- Fibroblast activity and extracellular matrix remodeling
- Controlled inflammatory signaling (not zero inflammation)
This is why Tβ4 is often discussed in the same breath as recovery and healing.
Aesthetics tie‑in: repair biology is anti‑aging biology In regenerative aesthetics, “anti‑aging” is not a cosmetic slogan. It is a tissue quality goal:
- Collagen organization
- Microcirculation
- Barrier function
- Faster recovery after aesthetic procedures
5) BPC‑157
What is BPC‑157 and why is it everywhere in sports recovery and GI conversations?
BPC‑157 (Body Protection Compound) is a synthetic peptide fragment derived from a gastric protein, widely discussed for:
- Tissue repair signaling (tendon/ligament narratives)
- Inflammation modulation
- Gastrointestinal protection concepts
What clinicians must be careful about BPC‑157 is a high‑interest peptide, but much of the enthusiasm is based on preclinical research and limited human data.
That doesn’t mean “ignore it.” It means:
- Separate mechanistic plausibility from clinical certainty
- Treat it as an evidence‑evolving area
- Build protocols around patient safety, quality control, and outcome tracking
Frequently Asked Questions (FAQ)
Are peptides safe? Safety depends on the specific peptide, indication, patient selection, and—critically—product quality and clinical monitoring. FDA‑approved peptide drugs have the strongest safety framework; other peptides may have limited human data.
Is semaglutide a peptide? Yes. Semaglutide is a peptide-based GLP‑1 receptor agonist used in metabolic medicine.
Can peptides help with skin aging? Some peptides are used in regenerative aesthetics because skin quality is influenced by inflammation, recovery capacity, microcirculation, and collagen remodeling biology.
Are CJC‑1295, Ipamorelin, BPC‑157, and Thymosin peptides FDA‑approved for anti‑aging? Many peptides discussed in longevity and recovery circles are not FDA‑approved for those uses. Clinicians should communicate evidence level, regulatory status, and safety monitoring clearly.
How does ISSCA approach peptide education? ISSCA focuses on mechanisms, evidence interpretation, patient safety frameworks, and regenerative protocols that connect metabolism, repair biology, and long-term outcomes.
Conclusion
Peptides are not a trend—they are a language of cellular communication. The five peptides highlighted here are popular because they map to the systems physicians work on every day: metabolism, immune regulation, recovery, tissue remodeling, and neuroendocrine balance.
The clinical advantage is not simply adding peptides to a menu. It is applying a regenerative strategy: selecting the right tool for the right bottleneck, tracking outcomes, and protecting patients with evidence-based decision-making.
If you want ISSCA to tailor this into a physician-facing guide, a patient-friendly blog version, or a landing page for your peptide certification funnel, tell me your target audience and CTA and I’ll adapt it.