Why are MUSE cells considered a new frontier in regenerative medicine?
Multilineage-differentiating stress enduring cells, commonly known as MUSE cells, represent a distinct population of endogenous stem cells that have attracted significant scientific interest over the last decade. First described by Professor Mari Dezawa and her research group in Japan, MUSE cells are naturally occurring, pluripotent stem cells found within adult tissues, offering a unique bridge between embryonic-like potential and adult stem cell safety.
Unlike embryonic stem cells or induced pluripotent stem cells (iPSCs), MUSE cells do not require genetic manipulation to express pluripotency. This characteristic positions them as a biologically conservative yet highly versatile cell population within regenerative medicine research.
What exactly are MUSE cells?
MUSE cells are a rare subset of mesenchymal stromal cells that express key pluripotency markers such as SSEA-3, while remaining non-tumorigenic. They reside in connective tissues throughout the body, including bone marrow, skin, adipose tissue, and internal organs, where they remain quiescent under normal conditions.
Under conditions of severe cellular stress—such as ischemia, inflammation, or tissue injury—MUSE cells become activated, migrate to damaged sites, and participate in tissue repair. This stress-responsiveness is one of their defining biological features and the origin of their name.
What does MUSE mean and why is stress important?
The term Multilineage-Differentiating Stress Enduring reflects the ability of MUSE cells to survive hostile microenvironments and differentiate into cell types derived from all three germ layers: ectoderm, mesoderm, and endoderm. Scientific studies have demonstrated that MUSE cells can integrate into injured tissue and differentiate in situ, responding to local biological cues rather than forced laboratory programming.
This stress-driven activation differentiates MUSE cells from other stem cell populations that often require ex vivo expansion or artificial induction.
How do MUSE cells work inside the body?
Once activated, MUSE cells follow chemotactic signals released by injured tissue. After homing to the damaged site, they can:
- Integrate into host tissue without forming tumors
- Differentiate according to the surrounding microenvironment
- Modulate inflammation and immune responses
- Support structural and functional tissue repair
Importantly, MUSE cells have demonstrated low immunogenicity, allowing them to evade immune rejection even in allogeneic research models. This property is supported by their expression profile and lack of strong MHC class II activation.
What medical conditions are being studied with MUSE cells?
Preclinical and early clinical research has explored MUSE cells in a variety of medical contexts. Published studies suggest potential roles in:
- Neurological injury, including ischemic stroke and spinal cord damage
- Chronic wounds and skin regeneration
- Myocardial ischemia and cardiac repair
- Liver and kidney fibrosis
- Inflammatory and autoimmune-related tissue damage
It is important to note that these applications remain within regulated research and clinical trial frameworks, and ongoing studies continue to define safety, efficacy, and appropriate indications.
How are MUSE cells different from traditional stem cells?
MUSE cells differ from other stem cell types in several clinically relevant ways. Unlike embryonic stem cells, they do not form teratomas. Unlike iPSCs, they do not require reprogramming or genetic modification. Compared to conventional mesenchymal stem cells, MUSE cells demonstrate broader differentiation capacity and intrinsic homing behavior.
This combination of pluripotency, safety, and biological responsiveness is what makes MUSE cells particularly compelling for regenerative medicine research.
Frequently Asked Questions (FAQ)
Are MUSE cells approved medical treatments?
MUSE cells are currently studied within regulated clinical research environments. Approval status depends on country-specific regulatory agencies.
Do MUSE cells replace stem cell therapies?
No. They represent a distinct stem cell population with unique properties that complement existing regenerative research.
Do MUSE cells cause tumors?
Published research indicates that MUSE cells are non-tumorigenic, unlike embryonic stem cells.
Why are MUSE cells considered important for the future of regenerative medicine?
Because they combine pluripotency, immune tolerance, and safety without genetic manipulation.
Conclusion
MUSE cells represent one of the most biologically intriguing developments in modern regenerative medicine. Their ability to endure stress, migrate to injury, differentiate naturally, and integrate safely into damaged tissue challenges traditional assumptions about stem cell therapy.
As research continues to evolve, MUSE cells may help redefine how medicine approaches tissue repair—not by forcing regeneration, but by supporting the body’s own intrinsic capacity to heal.
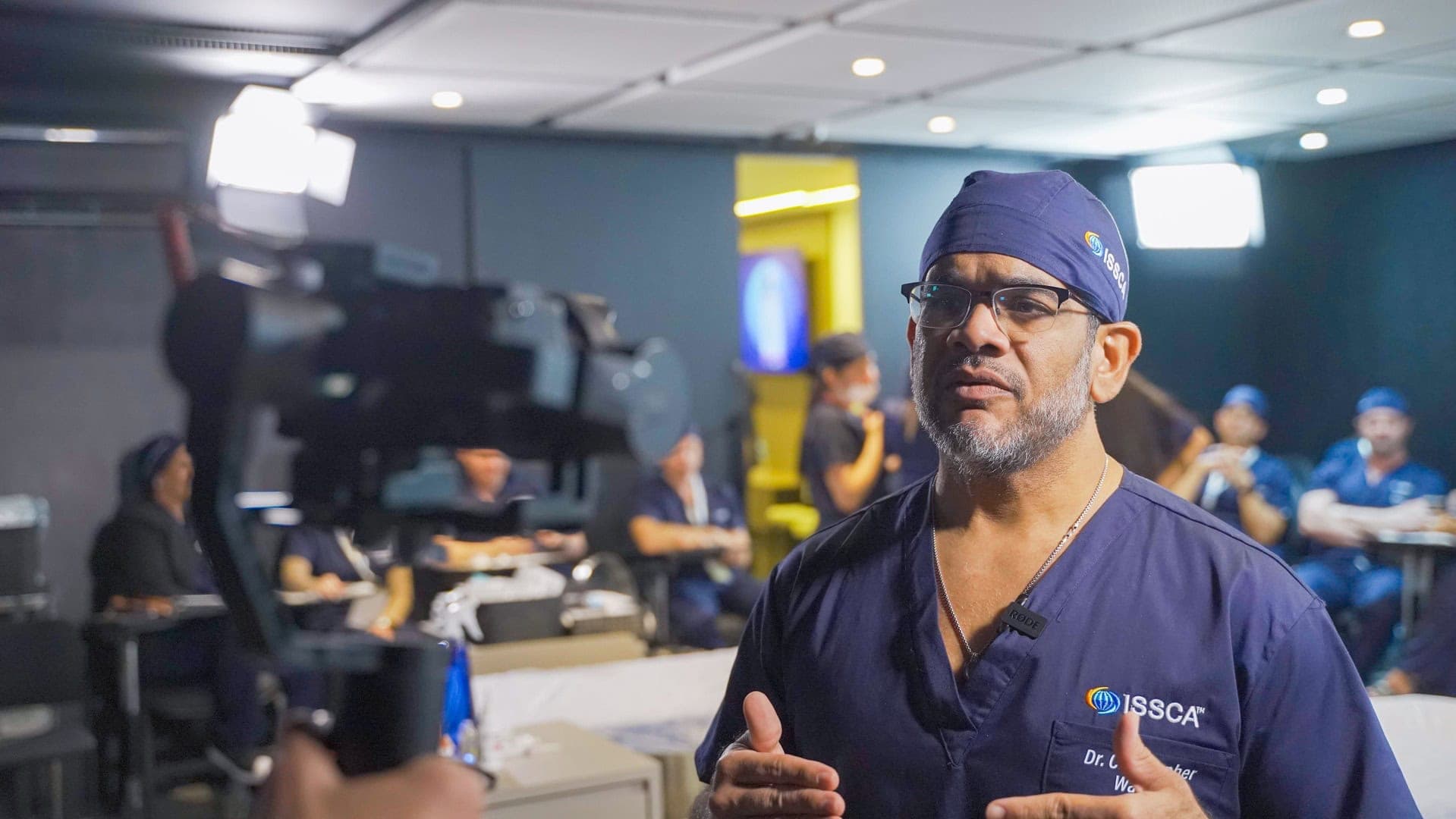
At ISSCA, MUSE cells are explored not as a promise, but as a scientific responsibility—rooted in evidence, ethics, and education.