Unlocking Multi-Organ Regeneration and Anti-Aging Therapies
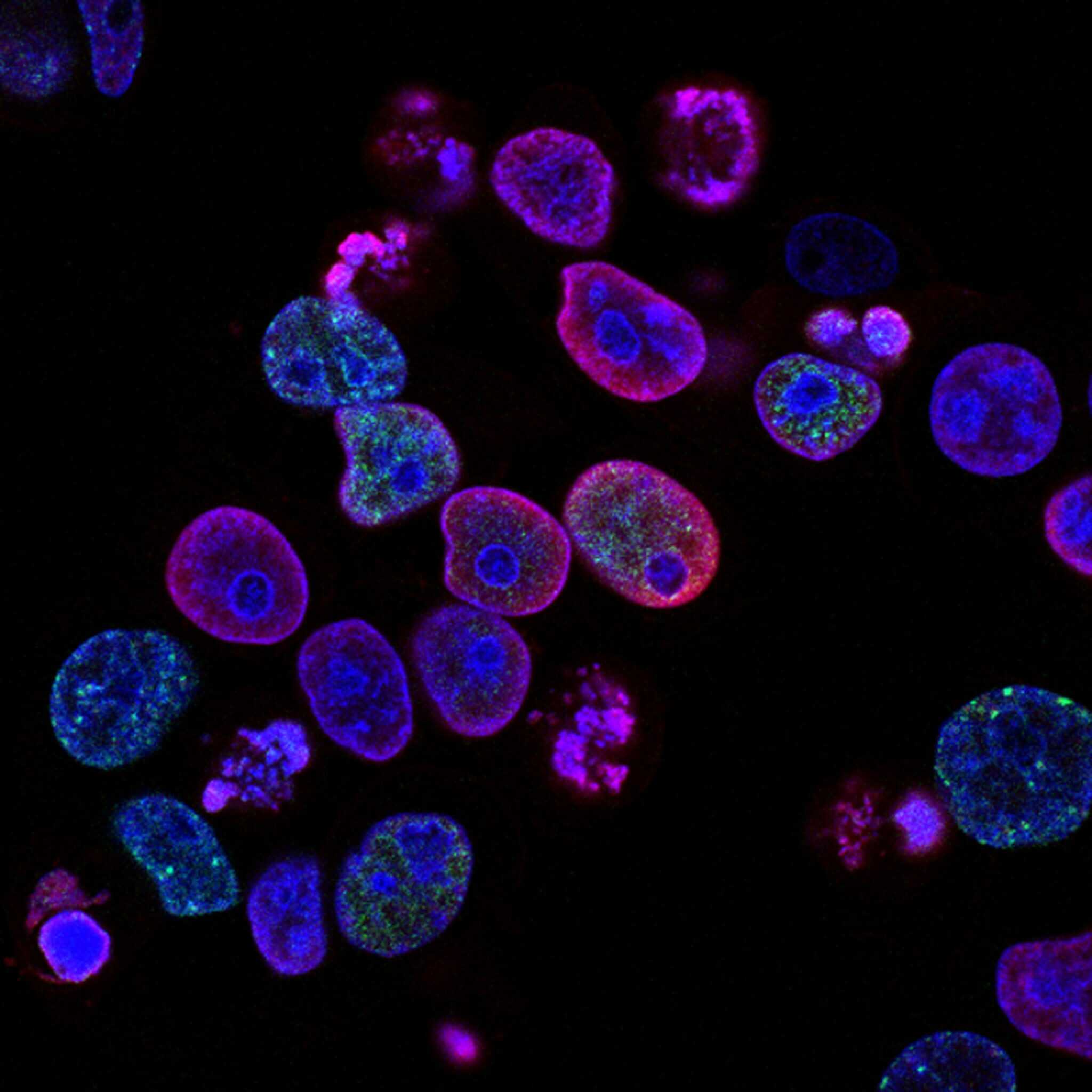
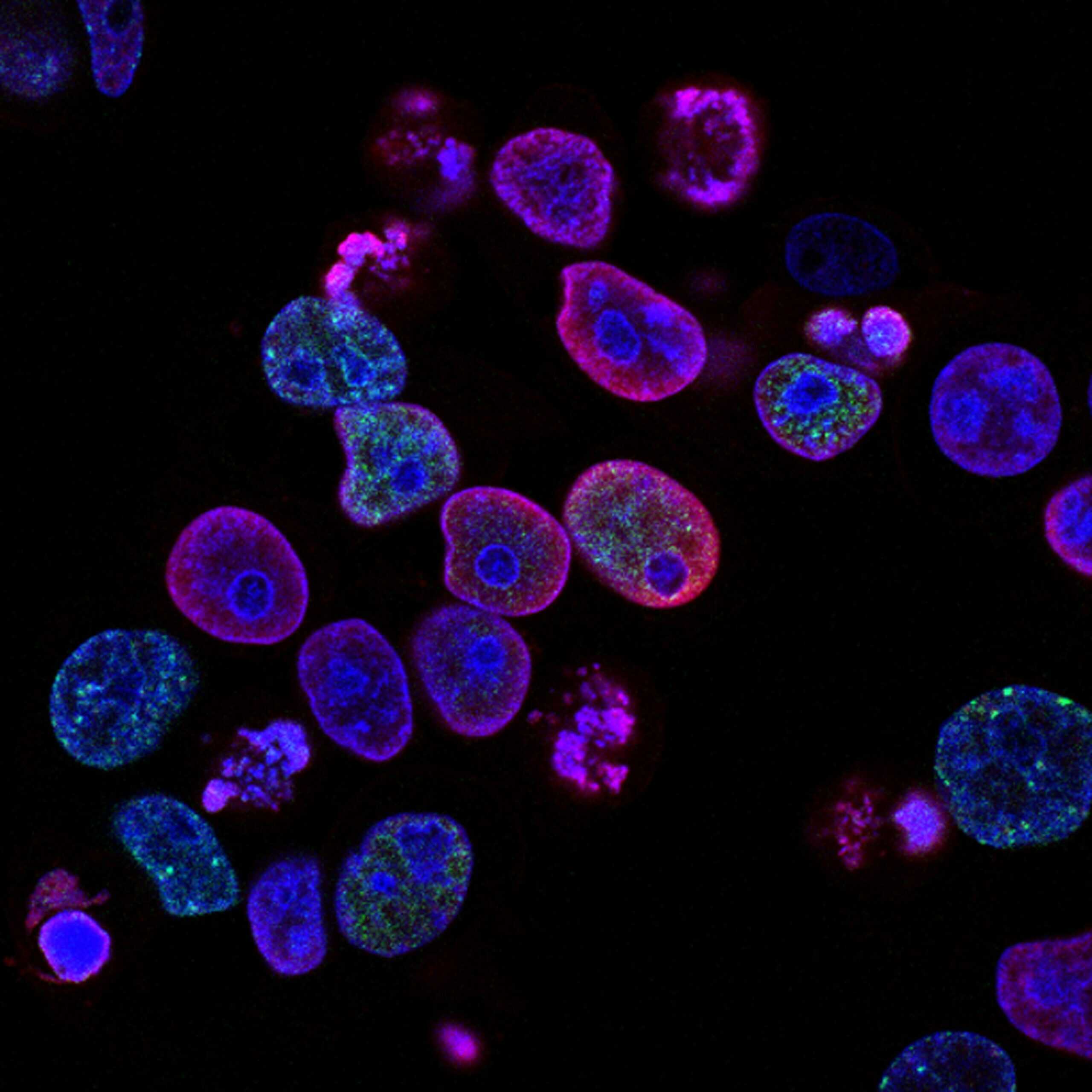
In the ever-expanding field of regenerative medicine, a unique discovery has redefined how physicians and researchers think about stem cells: Muse cells (Multilineage-differentiating Stress-Enduring cells). Unlike traditional stem cell populations, Muse cells combine the safety of mesenchymal stem cells (MSCs) with the regenerative breadth of pluripotent stem cells, offering a powerful tool for tissue regeneration and anti-aging cell therapy.
What Makes Muse Cells Different?
Muse cells emerged as a naturally occurring subpopulation within mesenchymal tissues. When exposed to extreme stress conditions such as hypoxia or serum deprivation, these rare cells not only survived but thrived.
Defining Characteristics of Muse Cells:
- Pluripotency markers (SSEA-3, Oct3/4, Nanog, Sox2) similar to embryonic stem cells.
- Mesenchymal lineage markers (CD105, CD90, CD73), confirming their MSC origin.
- Stress resilience, enabling survival in hostile microenvironments where most stem cells fail.
- Non-tumorigenic profile, eliminating concerns associated with embryonic or induced pluripotent stem cells (iPSCs).
This dual identity makes Muse cells a safe and versatile option for clinical translation.
Stress-Resistant Stem Cells for Real-World Medicine
The hallmark feature of Muse cells is their resistance to cellular stress. Unlike other stem cells that undergo apoptosis in inflamed or ischemic tissues, Muse cells remain metabolically active and functional.
This resilience has profound clinical implications:
- Stroke and spinal cord injury: Muse cells cross the blood–brain barrier and differentiate into neurons and glial cells.
- Myocardial infarction: Systemic administration leads to engraftment as cardiomyocytes, improving heart function.
- Liver disease: Muse cells integrate into hepatic cords, restoring liver enzyme profiles.
- Dermatology: In genetic disorders like epidermolysis bullosa, Muse-derived keratinocytes have demonstrated long-term tissue integration.
For regenerative physicians, this means Muse cells can be delivered intravenously—without complex surgical implantation—while still homing to damaged tissues.
Muse Cells in Anti-Aging Cell Therapy
Aging is characterized by cumulative cellular stress, chronic inflammation, and stem cell exhaustion. Muse cells uniquely counteract these drivers of degeneration through:
- Direct differentiation into functional neurons, cardiomyocytes, hepatocytes, and more.
- Paracrine signaling, releasing VEGF, HGF, and IL-10 to modulate the microenvironment.
- Senescence resistance, maintaining telomere length and avoiding premature aging markers.
These properties position Muse cells as a potential anti-aging therapy, capable of restoring tissue integrity across multiple organ systems. Unlike conventional stem cell therapies that rely heavily on paracrine effects, Muse cells provide both structural integration and immunomodulation, making them a powerful candidate for longevity medicine.
Clinical Evidence: From Bench to Bedside
While Muse cells are still early in their translational journey, several human studies and compassionate-use cases have shown encouraging results:
- Cardiac trials in Japan: Improved left ventricular function in patients with acute myocardial infarction following intravenous Muse therapy.
- Stroke patients: Demonstrated neurological improvement with MRI evidence of cell migration to peri-infarct regions.
- Genetic skin disorders: Integration of Muse-derived keratinocytes improved wound healing in epidermolysis bullosa patients.
These findings highlight Muse cells’ potential as one of the few stem cell types that combine pluripotency with safety—a critical factor for large-scale adoption in clinical practice.
Integrating Muse Cells into Regenerative Protocols
Muse cells are not meant to replace existing regenerative medicine protocols but rather to complement them. Their use alongside:
- Mesenchymal Stem Cells (MSCs): MSCs modulate immune responses while Muse cells directly regenerate damaged tissue.
- Exosomes: Rapid paracrine support from exosome therapy can prime microenvironments for Muse engraftment.
- Peptides and gene-modified therapies: Muse cells could be integrated into precision medicine strategies targeting organ-specific repair.
This integrative approach enhances outcomes, making Muse cells a multi-tool resource for regenerative physicians.
Challenges and Future Directions
As with any emerging therapy, challenges remain:
- Scalability: Muse cells are rare (~1–3% of MSC populations), requiring specialized isolation protocols.
- Regulatory clarity: Different jurisdictions are still determining whether Muse cells fall under minimally manipulated autologous use or advanced allogeneic therapy.
- Cost and accessibility: Manufacturing efficiency must improve for widespread adoption.
Future research is focusing on standardized GMP isolation methods, cryopreservation for off-the-shelf use, and large-scale randomized trials in neurology, cardiology, and dermatology.
Conclusion: A New Era of Multi-Organ Regeneration
Muse cells represent a paradigm shift in regenerative medicine. By combining the safety profile of mesenchymal stem cells with the pluripotency of embryonic-like cells, they offer physicians a practical and versatile option for tackling some of medicine’s most challenging conditions.
For clinicians in anti-aging cell therapy, tissue regeneration, and advanced clinical protocols, Muse cells could become a cornerstone of practice in the next decade.
At ISSCA, we see Muse cells not just as another stem cell discovery, but as the future of regenerative medicine—resilient, safe, and multi-lineage capable.