How did peptides move from basic biology to one of the most disruptive forces in modern medicine?
Over the past two decades, peptides have quietly reshaped multiple areas of clinical practice. Once viewed primarily as laboratory tools or niche hormones, peptides are now central to some of the most significant medical advances in metabolism, endocrinology, immunology, oncology, regenerative medicine, and aesthetics.
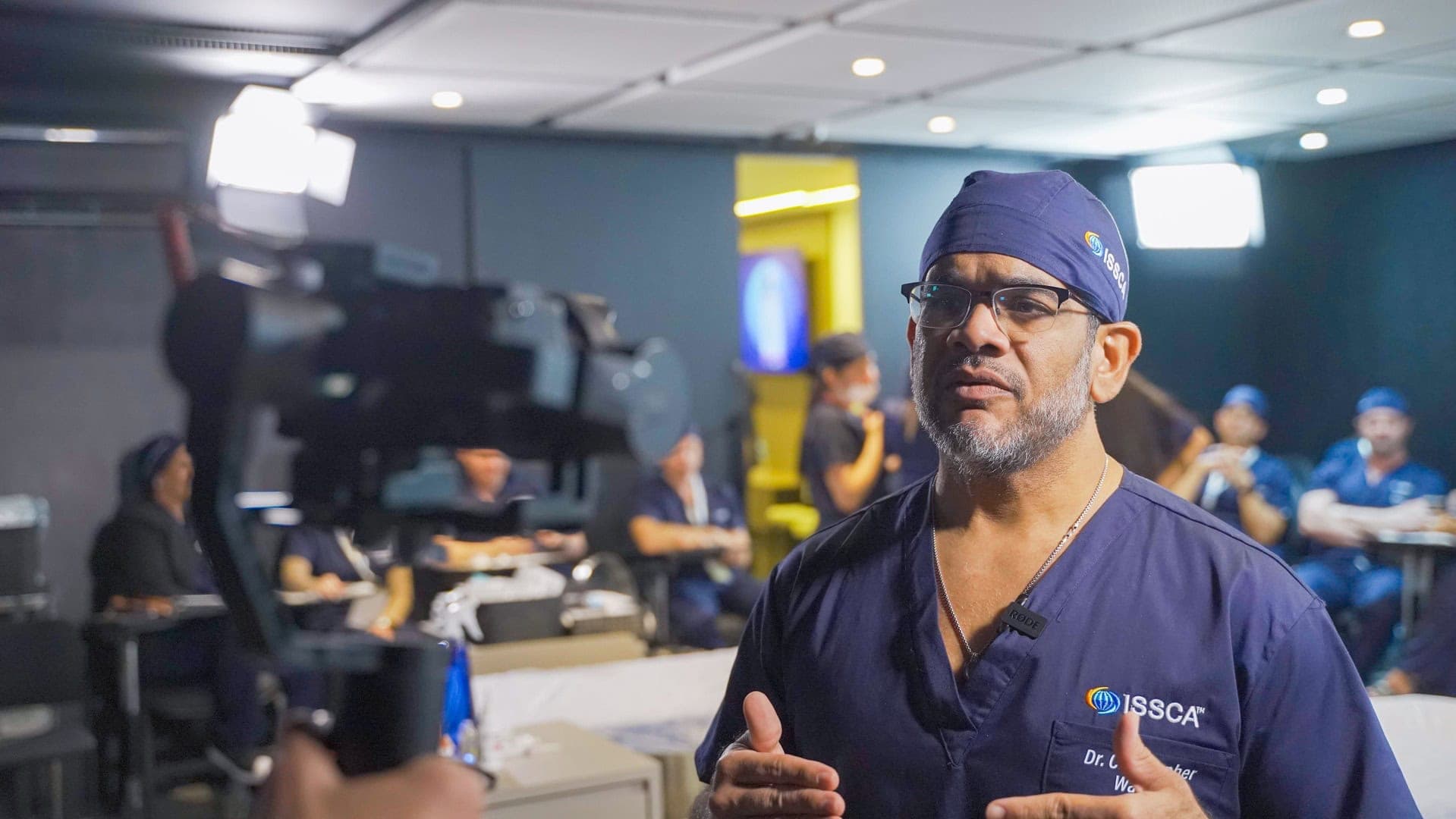
This transformation is not theoretical. It is reflected in FDA‑approved peptide drugs, large‑scale clinical trials, and a rapidly expanding body of peer‑reviewed research. From an ISSCA perspective, peptides represent a shift away from blunt pharmacologic force toward precision signaling medicine.
*Clinical note: This article is educational and does not provide dosing, compounding instructions, or treatment recommendations.
How peptides changed metabolic and obesity medicine
One of the most visible medical shifts driven by peptides has occurred in metabolic disease and obesity treatment. GLP‑1 receptor agonists, which are peptide‑based drugs, have fundamentally altered how clinicians approach weight loss, insulin resistance, and cardiometabolic risk.
Large randomized clinical trials published in journals such as The New England Journal of Medicine have demonstrated that GLP‑1 peptides can significantly reduce body weight, improve glycemic control, and lower cardiovascular risk markers. These findings reframed obesity from a purely behavioral issue into a hormonal and neuroendocrine condition amenable to biological intervention.
This shift has influenced not only endocrinology, but also preventive medicine, cardiology, and longevity science.
How peptides transformed endocrinology and hormone signaling
Peptides play a foundational role in endocrine regulation. Many of the body’s most important hormones—such as insulin, glucagon, growth hormone–releasing hormone, and gonadotropin‑releasing hormone—are peptides.
Advances in peptide engineering have allowed clinicians and researchers to:
- Mimic natural hormone pulses more accurately
- Improve receptor specificity and reduce off‑target effects
- Extend peptide half‑life for therapeutic use
Clinical research in endocrinology has shown that peptide‑based therapies can restore signaling pathways rather than simply replacing hormones, representing a conceptual shift toward signal optimization instead of hormone substitution.
Peptides and the evolution of immune modulation
Another major medical shift driven by peptides is the evolution of immune modulation. Rather than broadly suppressing or overstimulating the immune system, peptide research has focused on restoring balance.
Thymic peptides and immune‑regulatory peptides have been extensively studied in immunology literature for their ability to influence T‑cell maturation, cytokine signaling, and immune tolerance. Clinical studies published in immunology and infectious disease journals suggest that peptides can support immune resilience without the collateral damage associated with aggressive immune suppression.
This approach has influenced how clinicians think about chronic inflammation, autoimmune conditions, and immune aging.
The role of peptides in oncology and targeted therapies
Peptides have also driven important changes in oncology. Peptide‑based targeting strategies are used in cancer diagnostics, imaging, and drug delivery systems.
Research published in oncology and molecular medicine journals has demonstrated that peptides can:
- Bind selectively to tumor‑specific receptors
- Improve drug targeting while reducing systemic toxicity
- Enhance imaging precision for cancer detection
These developments contributed to the broader movement toward precision oncology, where treatments are tailored to molecular characteristics rather than generalized cytotoxic approaches.
How peptides reshaped regenerative medicine and tissue repair
Regenerative medicine represents one of the most profound areas of peptide‑driven change. Peptides involved in cell migration, angiogenesis, extracellular matrix remodeling, and wound healing have been studied extensively in tissue repair research.
Scientific literature in regenerative biology shows that peptides can influence:
- Fibroblast activation and collagen remodeling
- Vascular growth and microcirculation
- Controlled inflammatory signaling during healing
These discoveries shifted regenerative medicine away from purely structural interventions and toward biological environment optimization, where tissue repair is guided rather than forced.
Peptides and the medicalization of aesthetics
Aesthetic medicine has undergone its own transformation through peptide science. What was once focused primarily on volume replacement and surface correction is increasingly informed by skin biology, inflammation control, and tissue regeneration.
Dermatology research has demonstrated that certain peptides can stimulate collagen synthesis, improve dermal thickness, and support barrier function. This evidence helped redefine aesthetic anti‑aging as a regenerative process, not merely a cosmetic one.
As a result, aesthetic medicine is now closely linked to metabolic health, immune balance, and recovery capacity.
Why peptides represent a paradigm shift rather than a trend
The most important medical change driven by peptides is conceptual. Peptides changed how medicine thinks about intervention. Instead of overwhelming biological systems, peptide‑based therapies aim to communicate with them.
This paradigm shift is characterized by:
- Greater receptor specificity
- Improved safety profiles when appropriately used
- Alignment with endogenous physiology
- Integration with personalized and preventive medicine
These principles are now foundational to modern regenerative and longevity‑focused care.
Frequently Asked Questions (FAQ)
Are peptides widely used in mainstream medicine today?
Yes. Many FDA‑approved drugs are peptide‑based, particularly in endocrinology and metabolic medicine.
Do peptides replace traditional pharmaceuticals?
No. Peptides complement existing therapies and often improve precision and safety when used appropriately.
Is peptide medicine evidence‑based?
Some peptide applications are strongly supported by large clinical trials, while others remain emerging fields requiring further research.
Why are peptides important for the future of medicine?
Because they allow targeted, physiology‑aligned intervention rather than broad systemic disruption.
Conclusion
Peptides have driven some of the most important medical changes of the last two decades, from obesity and endocrinology to immunology, oncology, regenerative medicine, and aesthetics. Their impact lies not only in specific therapies, but in how they reshaped medical thinking.
By prioritizing signaling, precision, and biological cooperation, peptides helped move medicine toward a more regenerative, personalized, and sustainable future. At ISSCA, this evolution informs how physicians are trained to practice medicine that respects biology while advancing innovation.