The Expanding Role of MSCs in Regenerative Medicine
Mesenchymal stem cells (MSCs) have long been recognized as powerful tools for tissue repair, but recent research has revealed their broader role as immune modulators. In addition to regenerating damaged structures, MSCs can recalibrate immune responses, reduce chronic inflammation, and create a microenvironment that supports long-term systemic rejuvenation.
This dual function positions MSC therapy at the forefront of efforts to address not only localized injuries but also the underlying biology of aging and chronic disease.
Inflammaging: The Silent Driver of Age-Related Disease
Aging is not merely the passage of time—it is marked by a persistent state of low-grade inflammation, often termed inflammaging. This condition results from:
- Accumulation of senescent “zombie” cells releasing pro-inflammatory signals.
- Mitochondrial dysfunction producing excess reactive oxygen species (ROS).
- Dysregulated immune surveillance that fails to maintain homeostasis.
The consequences are profound, contributing to cardiovascular disease, osteoarthritis, neurodegeneration, and frailty. For regenerative medicine, addressing inflammaging is essential for extending both lifespan and healthspan.
Why Mesenchymal Stem Cells Are Uniquely Suited
Unlike pharmacological interventions that target one pathway, MSCs operate on multiple fronts:
- Cytokine modulation: Downregulating TNF-α, IL-6, and IL-1β while enhancing IL-10 and TGF-β.
- Immune cell reprogramming: Polarizing macrophages from pro-inflammatory (M1) to reparative (M2).
- Exosome secretion: Delivering microRNAs and proteins that suppress inflammation and promote angiogenesis.
- Senescence interference: Reducing the secretion of pro-inflammatory SASP factors from aged cells.
This multifaceted approach makes MSC therapy one of the few strategies capable of addressing the root causes of inflammaging.
Clinical Advances: Evidence of Systemic Rejuvenation
A growing body of preclinical and early clinical evidence demonstrates MSCs’ potential to restore systemic balance:
- In aged mice, MSC infusions reduced IL-6 and TNF-α, improving endurance and cognition.
- In osteoarthritis, intra-articular MSC injections lowered inflammatory markers and improved mobility.
- In COPD patients, intravenous MSCs improved lung function and decreased exacerbations.
- In metabolic syndrome, MSC therapy enhanced insulin sensitivity and reduced high-sensitivity CRP levels.
These findings reinforce MSCs’ role as anti-inflammatory agents with broad applications in regenerative medicine.
Practical Considerations for Physicians
To translate these findings into practice, clinicians must carefully consider:
- Cell source:
- Autologous MSCs minimize immune risk but may decline in potency with age.
- Allogeneic and perinatal sources (umbilical cord, Wharton’s jelly) provide more consistent potency.
- Autologous MSCs minimize immune risk but may decline in potency with age.
- Administration route:
- Intravenous infusions for systemic effects.
- Intra-articular injections for localized conditions.
- Intrathecal or intranasal delivery in specialized neurodegenerative protocols.
- Intravenous infusions for systemic effects.
- Adjunctive strategies: Nutritional support, peptides, and exosomes can enhance MSC efficacy and longevity of results.
From Chronic Disease Management to Preventive Longevity
One of the most exciting developments is the use of MSCs in preventive and anti-aging protocols. By treating inflammaging as a biomarker of biological age, regenerative physicians can intervene proactively, reducing the risk of degenerative diseases before they manifest.
Emerging models position MSC therapy not just as a “rescue treatment” but as part of annual rejuvenation programs, reframing it as a proactive tool for long-term health maintenance.
Future Directions in MSC Therapy
Advances on the horizon include:
- Precision MSC subtypes: Identifying cell populations with enhanced angiogenic, neuroprotective, or immunosuppressive properties.
- Exosome-based biologics: Cell-free products retaining much of MSCs’ functionality with easier storage and regulatory pathways.
- Combination therapies: MSCs paired with senolytics, peptides, or gene-modified platforms for synergistic outcomes.
- AI-driven personalization: Predicting patient response and optimizing treatment schedules through multi-omics profiling.
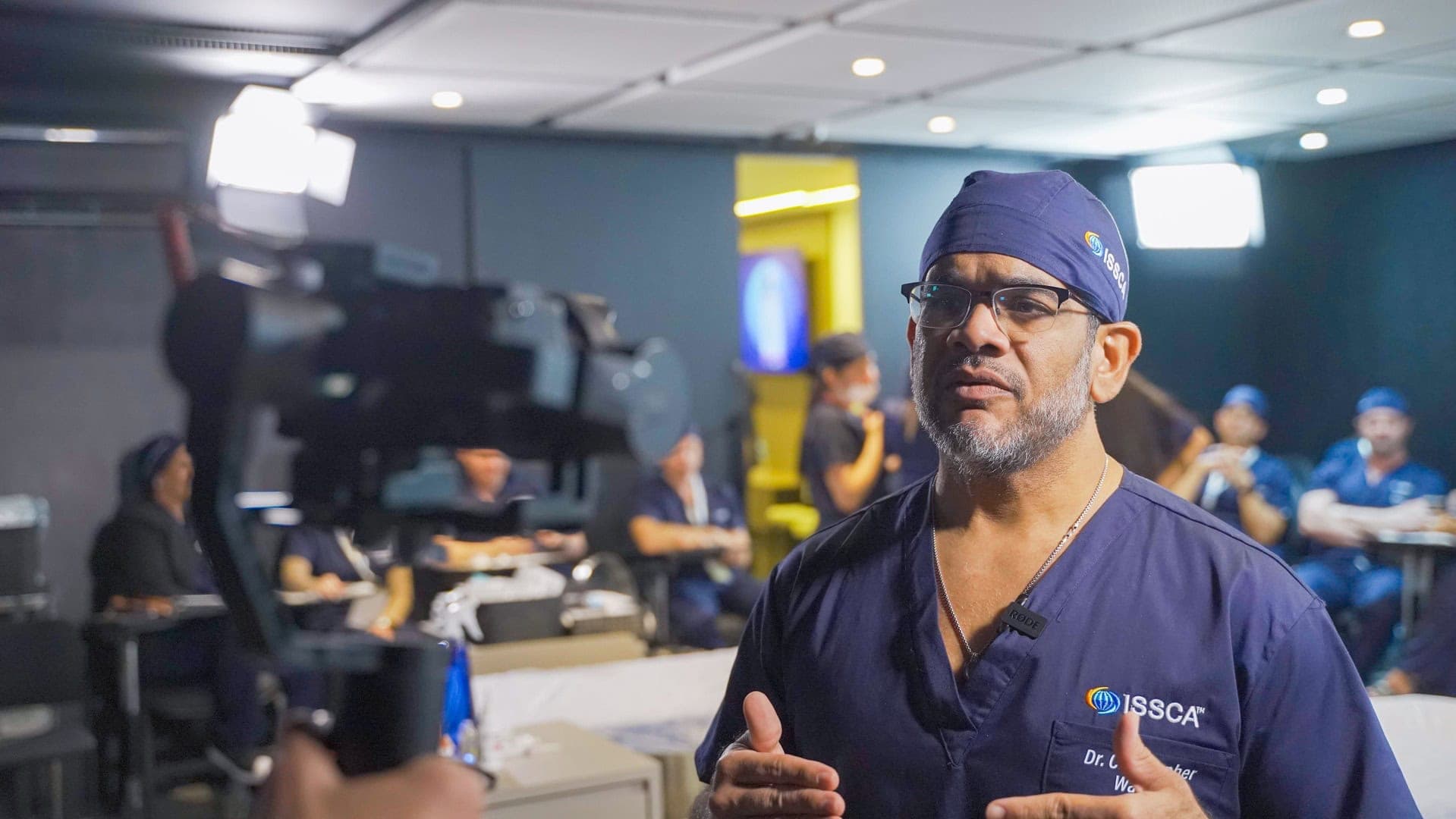
Conclusion: MSC Therapy as a Cornerstone of Regenerative Medicine
Mesenchymal stem cell therapy is rapidly evolving from experimental treatment to mainstream clinical intervention. By targeting the drivers of inflammaging and promoting systemic rejuvenation, MSCs offer physicians a powerful tool to address chronic disease and extend healthspan.At ISSCA, we view MSC therapy as a pillar of regenerative medicine protocols, providing physicians with the means to not only repair but also recalibrate the human body at its most fundamental level.